Dexcom has had my back (of my arm) for a few months now and it has gone really well. My anxiety has improved quite a bit now that I’m not constantly wondering what my blood sugar has been up to. While I wasn’t expecting that, what I was expecting was to find patterns to my blood sugar, and magically know how to address them…
ahem
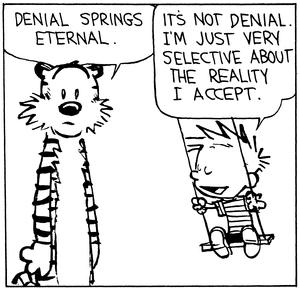
That has turned out to be a lot more difficult than I thought!
Some things I have pretty good control over, like noticing that I’m under-counting carbs, or timing my pre-bolus to better match my insulin action profile. But what I still really struggle with is my basal.
My blood sugar starts going up at night, even when I don’t eat, making bolusing for dinner confusing. Right now it’s 5:20, my blood sugar is 167, I haven’t eaten anything in 4 hours and my lunch was low-carb (and a small portion). Ugh! When I do eat dinner, my blood sugar spikes, come down nicely with my meal bolus only to rebound hours later, much higher than can be attributed to protein.
On the flip side, dawn phenomena is kicking my ass every morning. The inevitable rise begins at 2-3am, and by the time I wake up I need stupid amounts of insulin to bludgeon it back down. Even if it’s not too bad waking up “only” 150 or so, if I don’t correct, I’ll shoot over 200 as the morning goes on.
I’ve tried increasing my basal to amounts that I am just really uncomfortable with and I end up with lows in the afternoon. I want to keep my insulin at a minimum, but with MDI I just don’t have enough control to do so, and keep my blood sugar where it belongs.
This was a really long way to say that I am now the proud owner of an insulin pump! My endo thought it was a good idea, no convincing required, which was really nice. Just another confirmation that seeing someone who is used to T1’s is giving me better care, even though I’m a lowly T2.
I could go off on a rant about my insurance (UHC) only covering Medtronic, but the short story is that after looking at the pumps, I bought myself a Tandem t:slim X2. It can upgrade its firmware, so that next year when integration with my Dexcom G5 is ready, I can just download the update. They also are working on a hybrid closed loop system, which I am really excited to try.
I would have gone with the t:flex, which is large enough to hold three days of insulin, but Tandem isn’t planning on adding any of the great X2 features to it. So no CGM integration, no upgrading, no hybrid closed loop. Very disappointing to see that the latest technology isn’t available for the only T2 friendly pump, but unfortunately it’s not all that surprising either…
The pump arrived almost two weeks ago, but I’m still waiting for training. There’s been a bit of a hold up trying to get the pump settings from my endo, and Tandem won’t do the training without them. Being the dork that I am, I have already programmed it with some defaults gleaned from Pumping Insulin. But I’m not willing to piss people off by starting without training. Also I think help with my first infusion set, and getting a bunch of samples from the trainer, will be worthwhile.
I’ll report back on how things turn out. Wish me luck!